Common Postpartum Pains & How to Treat Them
Pains and aches after pregnancy are very common, and they tend to happen during the first six weeks after delivery — the postpartum period. If these pains last much longer or are more severe, something could be wrong, and you should call your doctor.
This section will find the most common postpartum pains, what causes them, and how to reduce the pain.
The best thing you can do before leaving the hospital is to discuss with your doctor the possible complications you may experience and how to manage them. Your ob-gyn will prescribe the proper medications and is the first person to call if you need assistance.
Here are common postpartum problems and treatments that can help [8].
General Soreness & Aching
After giving birth, the most common problems you can experience are pains and cramps all over your body — especially in the lower back, neck, hips, knees, and joints — due to the immense strain the body suffers during pregnancy and labor [1].
Water retention and the extra weight are usually the biggest culprits for this kind of pain, though labor can also cause muscle soreness.
This general soreness can last several weeks after delivery but is usually gone after a couple of days.
Common Treatments
Over-the-counter pain medications can help with general discomfort. If the pain is too severe or lasts longer than it should, your doctor can prescribe analgesics and suggest other ways to cope. Physical therapy, acupuncture, correct nursing positions, and heating pads can all be helpful in this situation.

Vaginal Pain & Bleeding
It is normal to continue bleeding for about six weeks after you give birth, as your body eliminates all the leftover blood and tissue from your uterus. This bleeding, called lochia, comes in stages and starts heavy but should taper off over time.
It is also common to experience vaginal inflammation and swelling for six weeks or more after a vaginal delivery.
If you experience heavy bleeding or pass large clots, you may be suffering from postpartum hemorrhage [2]. This may happen because your uterus didn’t contract correctly during labor, and you should talk to your doctor.
Common Treatments
Ice packs can help decrease vaginal pain and swelling within the first twenty-four hours. Over-the-counter medications like ibuprofen can help ease the discomfort.
Persistent vaginal and pelvic pain can become chronic and is actually quite common, so don’t hesitate to talk to your doctor if things still don’t feel “right” after a few months [5].
Nothing but time can speed up routine healing or make the bleeding stop. In case of hemorrhage, a blood transfusion can be necessary. You must immediately contact your doctor if there’s a drastic increase in blood or large clots. However, keep in mind that increased activity can cause you to bleed a little heavier.
Afterpains (Uterine Cramping)
Another recurring pain that you can experience is uterine cramps, caused by a process named involution, when the uterus repeatedly contracts, shrinking to its initial size [3].
These pains are usually triggered by breastfeeding and are stronger during the first few days postpartum.
Common Treatments
These cramps and contractions can be soothed using pain relievers such as ibuprofen, but you can also try breathing techniques, uterine massage, and heat [6]. It is also advised to keep your bladder empty and nurse more often. While nursing makes them more painful, it also speeds up the process, allowing you to get over this stage more quicker.

Swollen & Tender Breasts
Engorgement is when your breasts become larger, harder, and very tender. This process happens due to an excess of milk.
It starts a few days after giving birth and can last around three days if you are not breastfeeding and until the milk dries up. If you are breastfeeding, the discomfort goes away as soon as you nurse. Engorgement can happen at any point while breastfeeding if the milk builds up. Pumping or nursing can reduce discomfort, and sticking to a nursing or pumping schedule can minimize the risks.
Sometimes the ducts become clogged and cause an infection, known as mastitis, which causes burning pain. Mastitis can be incredibly painful but can usually be treated at home.
Symptoms of mastitis include:
- A painful lump in the breast, often hot to the touch
- Extreme pain when nursing
- Flu-like symptoms, including fever, chills, fatigue, and aches
- Nipple discharge
Another painful condition that accompanies breastfeeding is sore and cracked nipples. Though it’s uncomfortable (often an understatement) and there’s little that helps, it’s important to continue nursing to avoid mastitis.
Common Treatments
The best solution for this complication is to breastfeed more often, every one to two hours, if possible. Yes, breastfeeding is your life for the first month. Your doctor can prescribe you pain medication and anti-inflammatories, but you can also try applying cold packs, pumping, and wearing supportive bras.
If you think you have mastitis, try doing the following:
- Apply heat to the area or take a hot shower to reduce the pain
- Avoid wearing tight bras or shirts until it’s better
- Drink plenty of fluids
- Massage the lump to encourage milk flow
- Nurse or pump often (despite the pain, this is crucial!)
- Rest
See your doctor if you don’t feel better after 24 hours.
Specialized creams or lanolin can help heal cracked nipples, so ask your doctor for recommendations.

Constipation
Constipation discomfort is expected after birth and can happen for several reasons: hormonal changes, dehydration, use of analgesics or iron supplements, or pain in the perineal area [4].
It is also expected after a c-section since major surgeries disturb the digestive system’s functions.
Constipation usually resolves itself within a week after giving birth, or less if taking medications. You should call your doctor if you notice rectal bleeding, painful bulging in the vagina or perineum, rectal or stomach pain, or no bowel movements after a few days.
Common Treatments
Drinking lots of water and eating meals high in fiber will help you end your constipation naturally. You can also use stool softeners and start walking more as long as you feel capable and are cleared by your doctor.
Hemorrhoids
Hemorrhoids are another common complaint — as if there isn’t enough to deal with — due to the pressure from labor and can cause pain, swelling, and bleeding.
Common Treatments
There are many ways to treat hemorrhoids; sitz baths, drinking plenty of fluids, stool softeners, and applying witch hazel can help reduce the discomfort. Sitting on a pillow can take off some of the pressure. If the pain lasts more than a few days, contact your doctor.

C-Section Pains & Itching
C-sections are major abdominal surgeries, and the scars can be pretty painful for a couple of weeks, the first week being the worst. By week two, the area should feel much better, though it will likely itch once it starts healing. Still, this can also happen because of dry skin or an infection.
Along with the expected pain at the incision site, you may experience other discomforts, such as back pain, gas, or pain while going to the bathroom. The scar can sometimes even feel numb. All these symptoms should go away with time as your body adjusts and returns to normal.
See your doctor if you notice the following problems with your scar:
- A foul smell
- Fever over 100.4
- Increased pain
- It splits
- Oozing
- Redness, warmth, or swelling around the incision
Common Treatments
The doctor will have specific treatments and warnings depending on the type of incision and suture. Follow all instructions and call with any concerns or questions. In general, you should avoid most exercises (keep moving, though!) and take it easy until your doctor says it’s ok. Keep the scar clean, and make sure to go to all appointments.
To soothe an itchy scar, apply a small amount of sunburn cream. Using an icepack for 5-10 minutes can help as well.

Best Natural Pain Relievers for Postpartum Recovery
You can try some natural pain relievers if you are dealing with pain after pregnancy [8]. Still, you shouldn’t solely rely on these. Never ignore what your doctor recommends and prescribes over the following alternatives. If breastfeeding, be extra careful about what medications and herbs you use. Some can harm your milk supply or your baby [7].
Butterbur
Butterbur (Petasites hybridus) has been used for centuries for its ability to help heal wounds, improve migraines, and reduce fever and muscle spasms. Its active compounds activate TRPA1 channels, affecting pain and inflammation.
Gastrointestinal upset is a common side effect of its use.
It can interact negatively with non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen.

Ginger
Ginger is a plant root that can safely be used as a remedy for nausea and inflammation and strengthens the immune system and breast milk production. It is important to note that large amounts can promote bleeding, so you should discuss it with your doctor first.
Still, it is an excellent alternative to over-the-counter medicines, and you aren’t likely to experience any downsides. A simple ginger tea can alleviate cramps, headaches, and digestive issues and promote better circulation.

Turmeric
Using small amounts of turmeric in your dishes can reduce inflammation, improve digestion, alleviate body aches, and fortify the immune system. In the postpartum stage, it can be an excellent aide since it increases milk production and improves your mood.
It is best to ask your doctor before adding turmeric to your diet since it can stimulate bleeding.

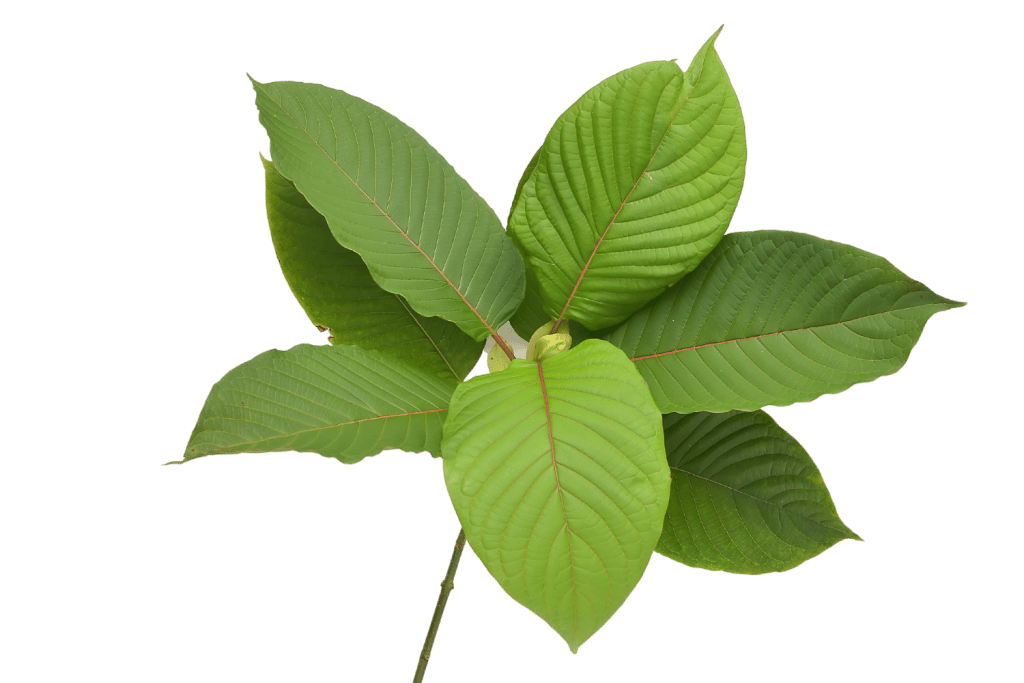
Kratom
Although kratom is not recommended for pregnant women, it is an option you may want to consider once you stop breastfeeding since it is one of the best natural analgesics available.
This herb has been a traditional remedy for centuries, serving as an excellent pain reliever and energy booster. However, using it when pregnant or nursing may be dangerous to your baby since it works similarly to opioids, so avoid it during this period.
Conclusion: How to Deal With Pain After Pregnancy
During the postpartum period, pains are to be expected. In most cases, they don’t require further treatment and will decrease with time — you should feel a lot better after the first few weeks.
Your doctor can prescribe the medications you need and recommend herbal products you can use for natural pain relief. If the pains persist or the symptoms worsen, you should seek immediate medical assistance. Never rely on alternative medicine not recommended by a professional.
- Miller, J. M., Low, L. K., Zielinski, R., Smith, A. R., DeLancey, J. O., & Brandon, C. (2015). Evaluating maternal recovery from labor and delivery: bone and levator ani injuries. American journal of obstetrics and gynecology, 213(2), 188-e1.
- Newsome, J., Martin, J. G., Bercu, Z., Shah, J., Shekhani, H., & Peters, G. (2017). Postpartum hemorrhage. Techniques in vascular and interventional radiology, 20(4), 266-273.
- Deussen, A. R., Ashwood, P., Martis, R., Stewart, F., & Grzeskowiak, L. E. (2020). Relief of pain due to uterine cramping/involution after birth. Cochrane database of systematic reviews, (10).
- Turawa, E. B., Musekiwa, A., & Rohwer, A. C. (2020). Interventions for preventing postpartum constipation. Cochrane Database of Systematic Reviews, (8).
- Paterson, L. Q., Davis, S. N., Khalifé, S., Amsel, R., & Binik, Y. M. (2009). Persistent genital and pelvic pain after childbirth. The journal of sexual medicine, 6(1), 215-221.
- El Sayed, S. L. M. (2021). Effect of uterine massage and emptying of the urinary bladder on alleviation of afterpains among mothers in the immediate postpartum period. International Journal of Africa Nursing Sciences, 15, 100327.
- Amer, M. R., Cipriano, G. C., Venci, J. V., & Gandhi, M. A. (2015). Safety of popular herbal supplements in lactating women. Journal of Human Lactation, 31(3), 348-353.
- Jahromi, B., Pirvulescu, I., Candido, K. D., & Knezevic, N. N. (2021). Herbal medicine for pain management: efficacy and drug interactions. Pharmaceutics, 13(2), 251.