Okay, let’s shift perspectives: imagine your body is a car, a high-performance speed machine, but there’s a catch. What if the ‘check engine’ light and ‘check oil’ light, basically all the indicators of automobile wear and tear, were broken? How would you know when something was wrong with the vehicle’s internal processes? If you receive no warning signs to stop or slow down, you’ll likely keep going.
This is the reality that people with congenital insensitivity to pain (CIP) live with every day. It is far removed from any illusion of superhuman ability; in fact, the condition can lead to many health problems.
What Is CIP?
Congenital insensitivity to pain (CIP) is a rare genetic disorder that affects the body’s ability to feel physical pain. Many people have it along with anhidrosis, or the inability to sweat (CIPA).

People with CIP are born unable to feel pain, heat, or cold and often have reduced or absent senses of touch and pressure. Although it may sound like a blessing, CIP can lead to serious health problems and complications, particularly in childhood when accidents and injuries are more common.
We’ll look closely at CIP, including its causes, symptoms, diagnosis, and management.
Causes of CIP
CIP is an extremely rare Mendelian genetic disorder caused by quirks in the genes that control the body’s ability to sense pain.
CIP is divided clinically into two groups — either the nociceptors fail to develop properly, or they develop but are not activated by pain signals [1].
The first group is Hereditary Sensory and Autonomic Neuropathies (HSANs), and HSAN4 is the most common cause of it. It’s common to see reduced cognition, susceptibility to Staphylococcus aureus infections, osteomyelitis, and septic arthritis.
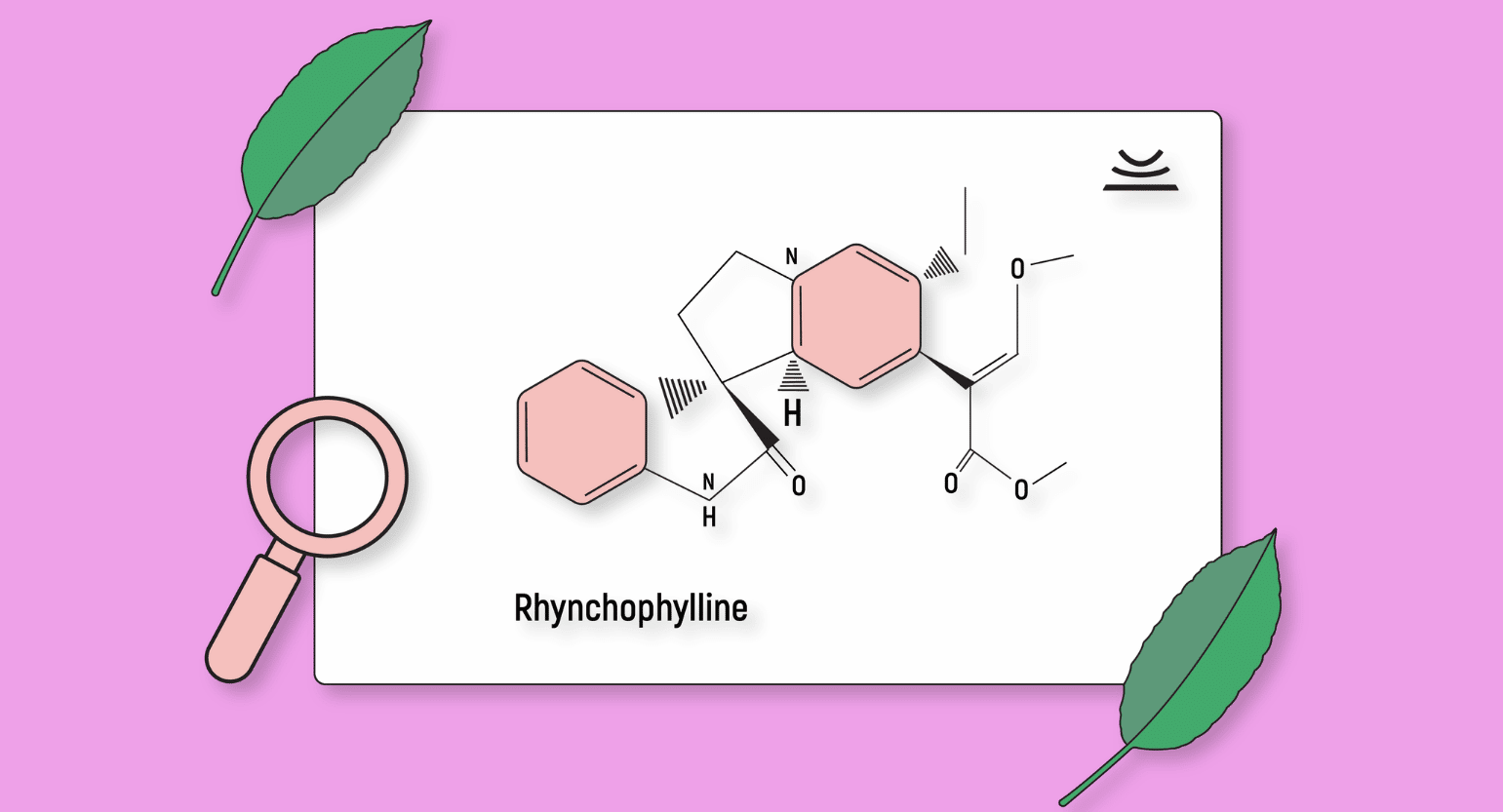
The second group is due to the nociceptor receptors’ inability to be activated by signals warning of tissue damage. The most common type is due to the gene SCN9A, or CIP-SCN9A (also called channelopathy associated with CIP). Cognition is normal, and there is no increased risk of staph infection, but there will often be congenital anosmia (absence of the sense of smell).
Other genes cause CIP phenotypes; most are autosomal recessive disorders.
Neurotrophic tyrosine kinase gene 1 (NRTK1) was the first gene identified as a cause of CIP and encodes for the protein TRKA.
Studying CIP has allowed researchers to understand pain pathways more clearly [2]. SCN9A and TRKA are being targeted for new analgesic treatments since those with SCN9A-CIP don’t feel neuropathic or visceral pain and have no cardiac, neurological, or cognitive deficits.
Does This Mean CIP Is Hereditary?
CIP is inherited in an autosomal recessive pattern. This means a person must have two copies of the gene — from both parents — to develop the condition.
If both parents are carriers of the CIP gene, each of their children has a 25% chance of inheriting the disorder [3]. CIP gene carriers have one regular, and one mutated copy of the gene and do not typically express symptoms of the condition.
Carriers can pass the mutated gene to their children despite the lack of symptoms.
Genetic counseling can help future parents understand the risk of passing on the CIP gene and make informed decisions about family planning.
Problems Associated With CIP
This rare genetic condition is characterized by the inability to feel pain, heat, or cold, making it impossible to recognize injuries, infections, or other health problems. Symptoms emerge very early in life and can be mitigated with medical attention.
Here is a rundown of the most common problems due to CIP [4, 5]:
Reduced or Absent Senses of Touch & Pressure
People with CIP may have limited or entirely absent senses of touch, and they cannot feel pressure. This hinders their ability to sense their limbs’ and body’s position and movement.
Increased Risk of Injuries
People with CIP are at a higher risk for injuries and health problems, particularly in childhood, when carefree exploration and play can lead to accidents and injuries.
For example, those who cannot feel pain may not realize they have a broken bone or a burn until it has become very severe or life-threatening.
Self-Mutilation
This is seen often, especially in children. Missing fingertips and mouth injuries are common.
Dental Problems
People with CIP may be at higher risk for dental problems, as their bodies dodoes not register the pain associated with tooth decay or gum disease.
Joint & Bone Problems
People with CIP are more likely to develop joint and bone problems since they don’t notice the strain of injured muscles. Charcot joints — the progressive decline of bone and soft tissues at weight-baring joints — are common.
Eye Injuries
Corneal reflexes are often absent, putting the eyes at risk for injury and permanent scarring.

Infections
People with CIP may be at higher risk for infections, as they may not feel it when they get cuts, scrapes, or other injuries.
Reduced or Absent Sweating
Those with CIP often sweat in negligible amounts or do not sweat at all, hindering the body’s ability to osmoregulate.
Here is a more comprehensive list of symptoms of CIP. Reading blog posts is not recommended as a tool for self-diagnosis but rather as a guide to understanding the condition.
Diagnosing CIP
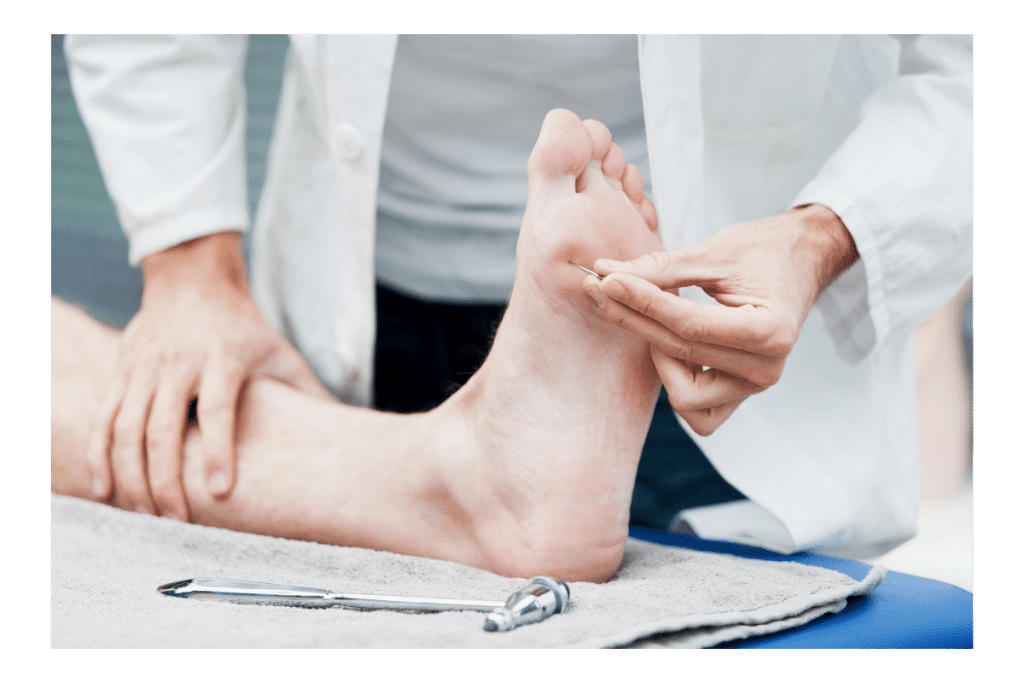
CIP is diagnosed through a combination of the following [5]:
- Clinical evaluation – This involves a thorough physical examination and a review of the patient’s medical history and symptoms.
- Genetic testing – A thorough analysis of a person’s DNA to identify any mutations in the SCN9A gene or other genes associated with CIP.
- Nerve conduction studies – Measuring the electrical signals traveling along the nerves to determine if they function correctly.

Is There Any Medication or Cure for CIP?
At present, there is no medication or cure for this condition. Symptom management involves regular monitoring for injuries or other health problems, physical therapy to improve muscle strength and coordination, and protective measures to prevent injuries.
It’s essential to work with a healthcare provider to develop an individualized treatment plan that meets each person’s specific needs in dealing with CIP.
While there is no cure for CIP, ongoing research will help us better understand the condition and develop new treatments or therapies that may help manage its symptoms.
Can You Use Kratom With CIP?
People with CIP often show signs of hyperactivity and emotional instability, so kratom could be calming and help with any anxiety or depression they’re dealing with.
However, the risks associated with kratom use may outweigh any potential benefits. Because everyone’s situation is different and there’s so little research available, consult your doctor if you have CIP and want to try kratom.

Does CIP Lower Life Expectancy?
Yes, due to how dangerous CIP is, those with it are not expected to live over 25 [6].
Overall, life expectancy is influenced by various factors, including other health conditions or complications and access to appropriate care and management.
Managing CIP
Although there is no cure for CIP, several strategies can help manage the symptoms and prevent complications.
Regular Checkups
A healthcare provider can check for injuries or emerging health problems that may or may not be related to CIP.
Physical Therapy
Physical therapy can help improve muscle strength and coordination and prevent joint and bone problems.
Protecting Oneself
People with CIP need to take extra care to protect themselves from injuries. This may include wearing protective gear, avoiding dangerous activities, and taking precautions when handling hot or sharp objects.
This also means constantly checking for cuts, sores, and other signs of injury, infection, or other health problems.
Dental Care
Regular dental checkups and good oral hygiene are essential for people with CIPA. They must be vigilant to prevent tooth decay and gum disease as they will not register the associated pain.

Managing Hydration
People with CIPA may find osmoregulating challenging because of their diminished ability to sweat. This can lead to overhydration or dehydration, both of which can prove harmful to their health. Therefore, maintaining a strict hydration schedule is critical.
Genetic Counseling
People with CIPA may benefit from genetic counseling, which can provide information about the condition and whether they can pass it on to their offspring. Such consultations will help families make informed decisions about their future.
Naloxone
Research shows naloxone can reverse the analgesia in some CIP patients, allowing them to feel pain.
One study tested naloxone on a person with CIP due to a lack of Nav1.7. Mutations of these sodium channels cause a functional absence of nociceptors. Before the patient was given naloxone under baseline conditions and with a saline placebo, they were unaware of noxious heat stimulus. After receiving 12 mg of naloxone, their ability to feel the heat stimulus rose to 80%, almost reaching the levels of healthy controls in the study. The patient also felt pain in one leg that had suffered multiple fractures [6].
While this is helpful for research purposes and in understanding how pain works, it also helps CIP individuals feel sources of pain, narrowing down any health issues. Doctors rely on symptoms to help find the correct diagnosis. If a person can’t feel discomfort, it’s hard to determine what needs attention and the source of any issues.
In Conclusion: Life With CIP
CIPA is a rare genetic disorder that affects the body’s ability to feel physical pain. It can lead to serious health problems and complications, particularly in childhood when accidents and injuries are more common.
Although there is no cure for CIPA, several strategies can help manage the symptoms and prevent complications, including preventive measures, pain management techniques, physical therapy, dental and bone care, and infection prevention.
- Drissi, I., Woods, W. A., & Woods, C. G. (2020). Understanding the genetic basis of congenital insensitivity to pain. British Medical Bulletin.
- Moraes, B. C., Ribeiro-Filho, H. V., Roldão, A. P., Toniolo, E. F., Carretero, G. P., Sgro, G. G., … & Schechtman, D. (2022). Structural analysis of TrkA mutations in patients with congenital insensitivity to pain reveals PLCγ as an analgesic drug target. Science Signaling, 15(731), eabm6046.
- Indo, Y. (2020). NTRK1 congenital insensitivity to pain with anhidrosis.
- Masri, A., Shboul, M., Khasawneh, A., Jadallah, R., ALmustafa, A., Escande-Beillard, N., … & Reversade, B. (2020). Congenital insensitivity to pain with anhidrosis syndrome: a series from Jordan. Clinical neurology and neurosurgery, 189, 105636.
- Schon, K. R., Parker, A. P. J., & Woods, C. G. (2020). Congenital insensitivity to pain overview. GeneReviews®[Internet].
- AL-EZZİ, J. İ. Congenital insensitivity to pain with anhidrosis syndrome: A case report in Diyala province/Iraq. Pediatric Practice and Research, 10(3), 134-138.
- Minett, M. S., Pereira, V., Sikandar, S., Matsuyama, A., Lolignier, S., Kanellopoulos, A. H., … & Wood, J. N. (2015). Endogenous opioids contribute to insensitivity to pain in humans and mice lacking sodium channel Nav1. 7. Nature communications, 6(1), 8967.